Practical application of PK/PD principles
Integrating the MIC with the PK parameters peak, trough and AUC results in three PD targets for antibiotics

The dose-response curve is an underlying principle of pharmacology and pharmacodynamics. Once the target is met, a plateau is reached. Higher doses will not result in more rapid killing. In fact, as we will see, larger doses often lead to adverse effects.

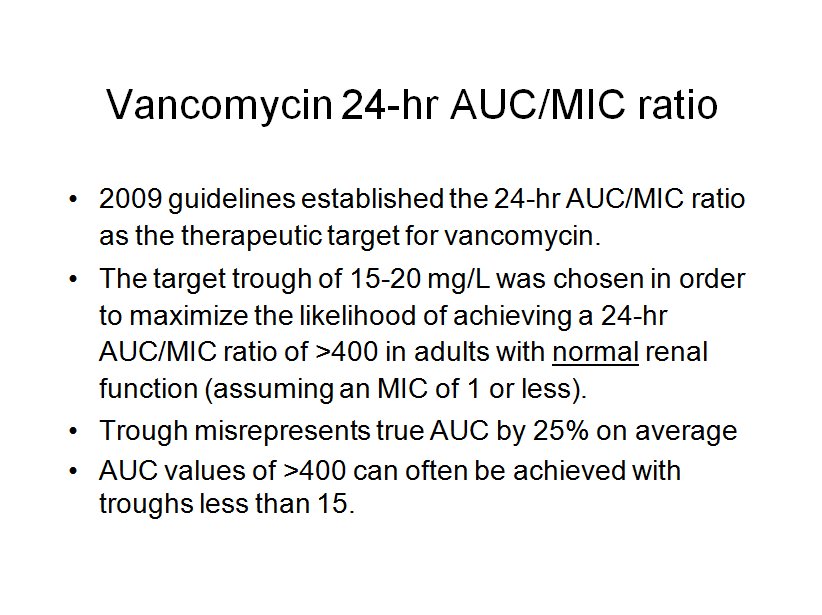
What was missed by many is the fact that the 2009 vancomycin consensus guidelines established the 24-hr AUC/MIC ratio as the therapeutic target. The trough goal of 15 to 20 mg/L was chosen as a surrogate marker for the true pharmacodynamic target, the AUC/MIC ratio.
There is a good deal of evidence that AUC/MIC ratio is the proper target for vancomycin dosing. The slide below is from a study of a mouse model of soft-tissue MRSA infection. Above the dotted line there is no inhibition. Below the dotted line there is increasing inhibition. Time Above MIC and Peak/MIC ratio are scatter plots. Looking at 24-hr AUC/MIC ratio a well defined pattern can be seen. At 100 or less there is no inhibition. At 200, most colonies are inhibited. At 400 or greater all colonies are inhibited. It is important to note that the higher ratio of 1000 did not result in more colonies inhibited. In other words, a response plateau was seen at 400.
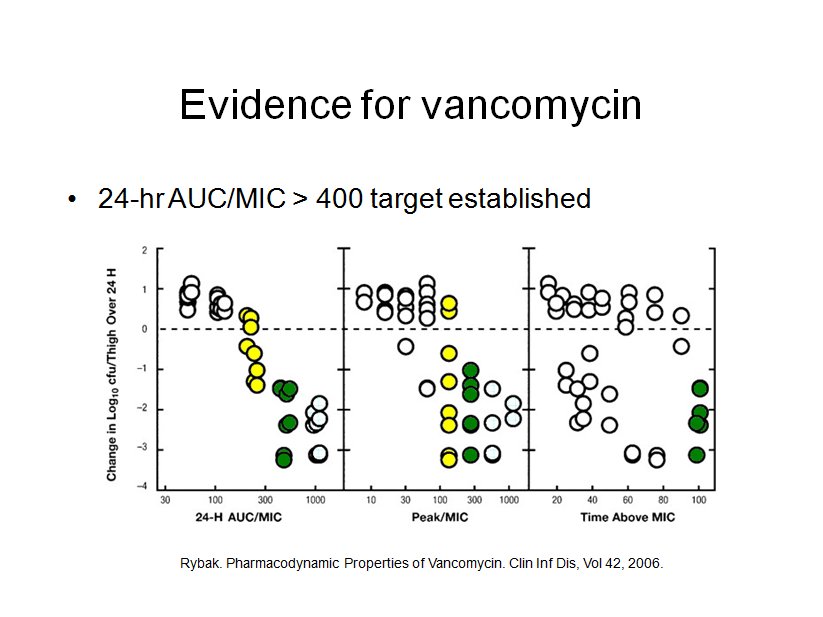
Numerous clinical studies have also established the suitability of the AUC/MIC ratio in predicting therapeutic efficacy.

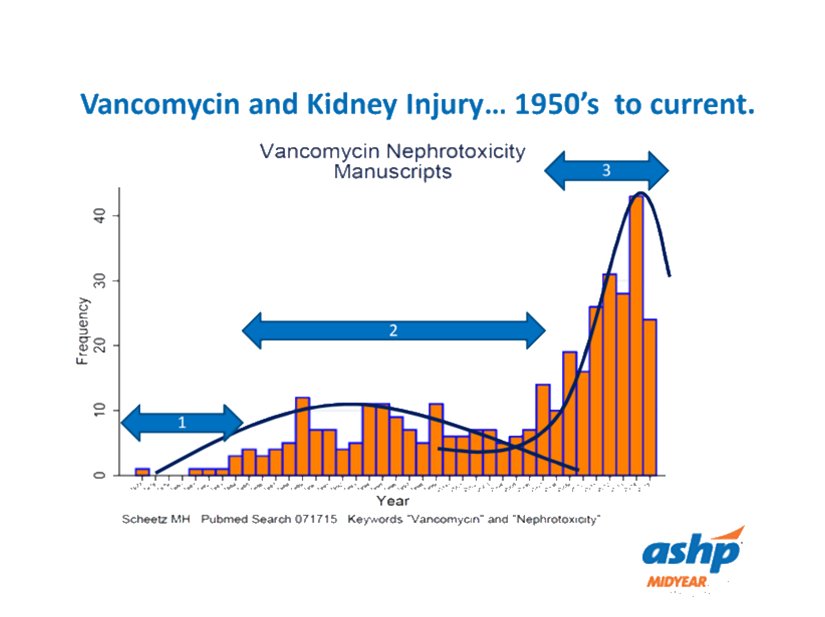
After the 2009 guidelines advocating higher trough levels came into widespread practice, the number of published reports of vancomycin associated nephrotoxicity skyrocketed.
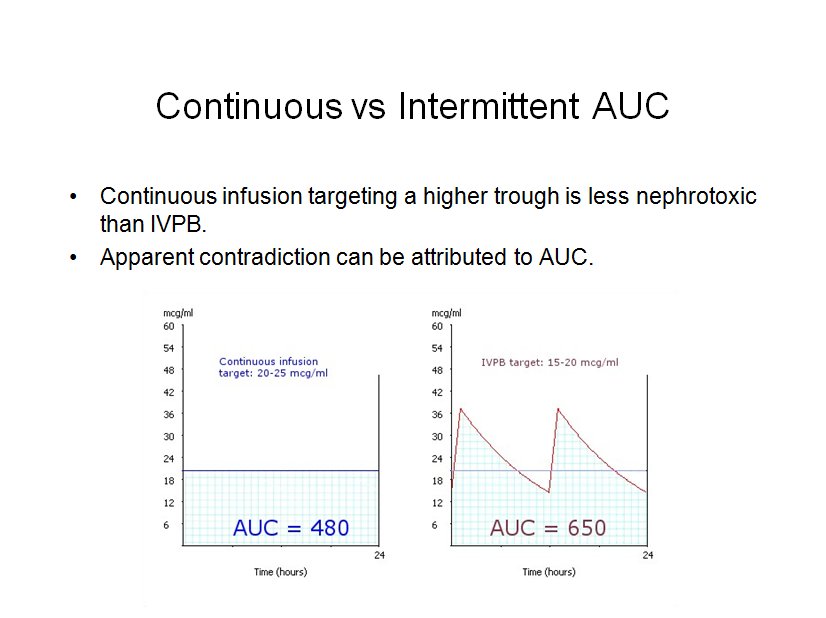
On the other hand, it has been clearly shown that a continuous infusion of vancomcyin, targeting a constant 20 to 25 mg/L, is less nephrotoxic than intermittent dosing targeting troughs of 15 to 20 mg/L. This apparent contradiction can be explained if we attribute the risk of nephrotoxicity to AUC, just as we do for efficacy.
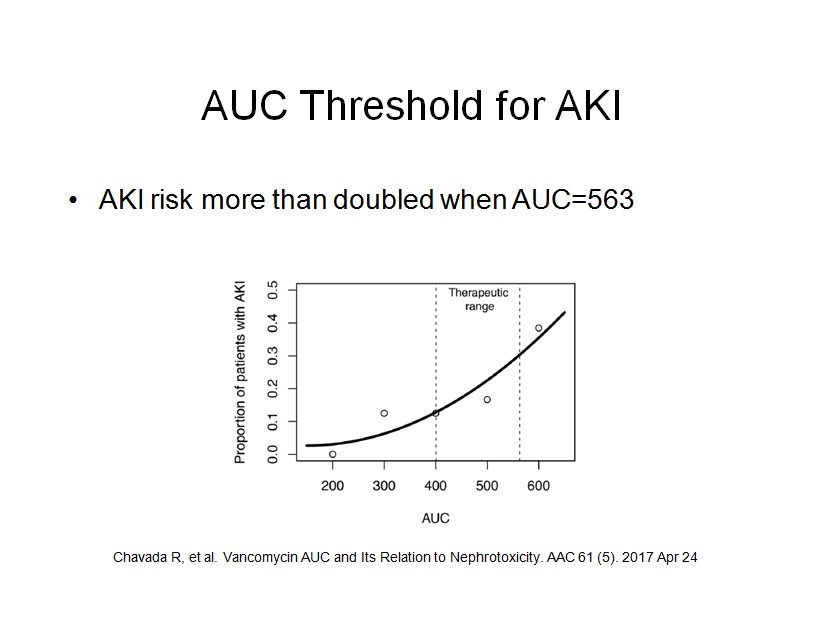
What is the AUC threshold for vancomycin associated AKI? The most often cited number in the literature is 600. In 2017 Chavada, et al. sought to answer this question. Theirs was a six year study of patients with bacteremia. They used a 1-compartment model, with AUC calculated from Bayesian analysis of a steady-state trough. They found that AKI risk more than doubled when the AUC exceeded 563.
The most widely used pharmacokinetic model for vancomycin is one-compartment. The equations for a one-compartment model are practical and time-tested. Because vancomycin exhibits a multi-compartment pharmacokinetic profile, the clinical application of the one-compartment model requires post-distribution serum samples. Also realize that the one-compartment model does not capture the distribution phase(s), and thus underestimates true peak by approximately 5 to 10 percent.
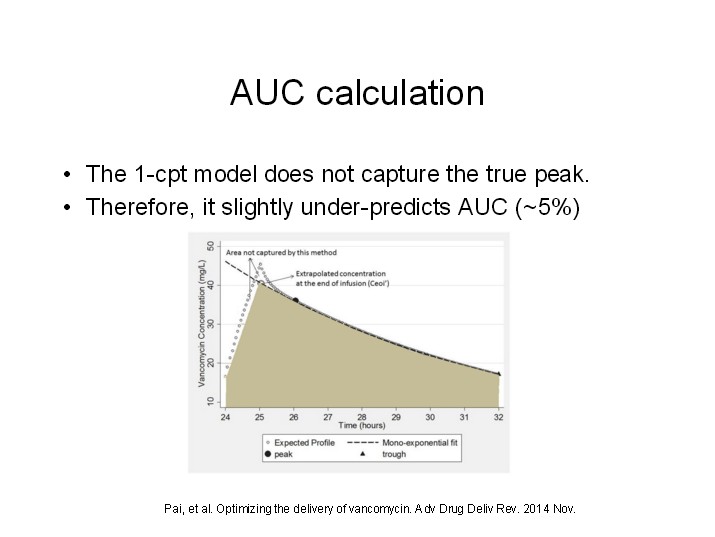
It is important to be cognizant of this AUC underestimation for two reasons. One, if the AUC calculated by our one-compartment model is 400, then you can be sure that you have hit the minimum AUC target. It follows that the maximum AUC should be less than 600. The study cited above by Chavada, which used a one-compartment model, found the AKI threshold to be 563, which is 6.1% less than 600.
Therefore, a safe and effective target AUC range for our one-compartment vancomycin model should be 400 to 550.
